Vulvar Cancer
Overview
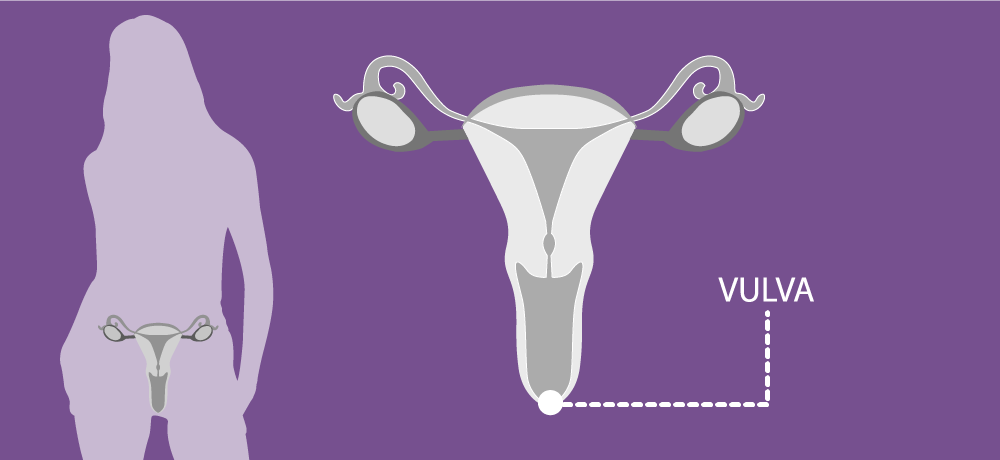
The vulva consists of several external organs, including the labia majora (outer lips), labia minora (inner lips) and clitoris, as well as the opening of the vagina and the urethra (the tube leading from the bladder).
Vulvar cancer is relatively rare, accounting for approximately 4% of all genital cancers in women. It is crucial to distinguish vulvar cancer from vaginal cancer, as both are distinct yet related to the female genital area.
Historically viewed as a cancer affecting post-menopausal women, vulvar cancer has seen a shift in age of onset. Recent years have marked a decline in the mean age of diagnosis, largely due to an uptick in HPV infections globally. Women over 65 years old remain the most vulnerable to developing vulvar cancer. However, an increase in cases among younger women is becoming evident, potentially linked to rising rates of HPV infection and tobacco use.
In 2022, Europe ranks second in vulvar cancer incidence and mortality compared with other continents. In 2020, the Global Cancer Observatory and the International Agency for Research on Cancer reported 16,506 new cases of primary vulvar cancer in Europe, with 6,503 associated fatalities.
Geographically, the risk varies across Europe, with higher incidence rates in Eastern and Northern countries compared with Western and Southern in 2022. A 2017 epidemiological study spanning 13 high-income countries revealed a notable 14% rise in vulvar cancer incidence overall. This increase, however, was not uniform across all age groups. Women under 60 experienced a 38% increase in incidence, while no significant change was observed in women over 60.
For more information, download the ENGAGe brochure on Vulvar Cancer, Vulvar Self-Examination guide, HPV tests or Gynaecological cancers in Europe (2024 update).
Symptoms
Signs and symptoms of vulvar cancer may include:
- Itching that doesn’t go away
- Pain, soreness or tenderness
- Bleeding
- Skin changes, such as color changes or thickening
- A lump or wart-like growth on the vulva
- A burning pain when passing urine
Check out our vulvar self-examination guide and consult your doctors in case you spot any abnormalities.
Risk factors
The exact cause of vulvar cancer is unclear, but your risk of developing the condition is increased by the following factors:
- Older age
- Vulvar intraepithelial neoplasia (VIN) – where the cells in the vulva are abnormal and at risk of turning cancerous
- Persistent infection with certain versions of the human papilloma virus (HPV)
- Skin conditions affecting the vulva, such as lichen sclerosus
- Smoking
- HIV infection
Diagnosis
If you notice signs of vulvar cancer, ask your doctor about them.
The doctor will carry out a gynecological evaluation, which includes checking the vulva and the vagina, if needed.
The examination should include the perineal area, including the areas around the clitoris and urethra.
If there is an ulceration, lump, or a mass that looks suspicious, then they will perform a biopsy. Local anesthesia may be used.
Depending on the results of the biopsy, there may be further tests:
- Cystoscopy: the bladder is examined to determine whether the cancer has spread to that area.
- Proctoscopy: the rectum is examined to check whether the cancer has spread to the rectal wall.
- Imaging scans: these can help the doctor determine whether the cancer has spread, and if so, where to. An MRI, CT and PET/CT scans may be used. An ultrasound scan is generally used to assess if there are any enlarged/suspicious groin lymph-nodes.
Treatment
The main treatments for vulvar cancer are:
- Surgery – In most cases, your treatment plan will involve some form of surgery.
- Chemotherapy – It’s usually used if vulval cancer comes back or to control symptoms when a cure is not possible.
- Radiotherapy – It can be used to relieve symptoms and improve quality of life.



