Uterine (Endometrial) Cancer
Overview
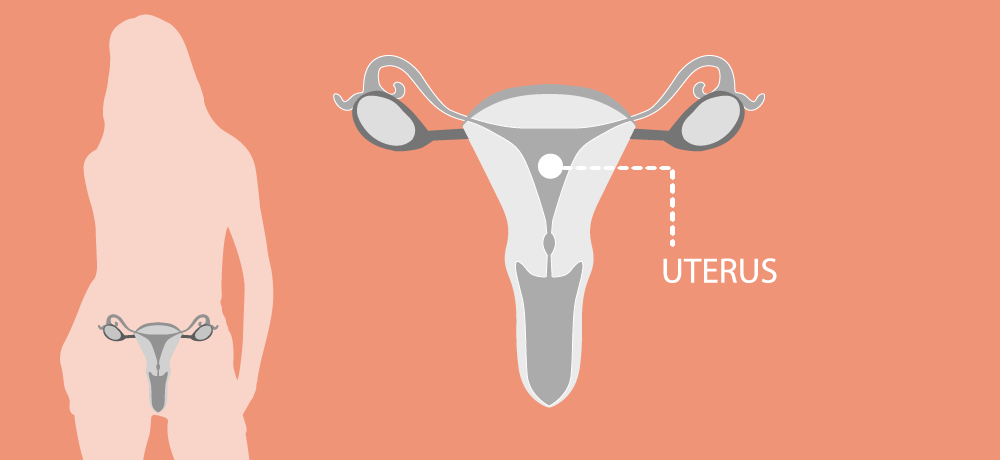
The uterus, also known as the womb, is where a fetus develops during pregnancy. This hollow, muscular organ, connected to the cervix, comprises three distinct layers. The innermost layer, the endometrium, is primarily responsible for preparing to host a fertilized egg. Each month that fertilization doesn't occur, a menstrual period is triggered and the superficial part of the endometrium is shed.
While there are various uterine cancers, the majority originate in the cells of the endometrium. These cancers, known as endometrial adenocarcinomas, develop from the lining of the womb. The terms ‘uterine cancer,’ ‘endometrial cancer’ and 'womb cancer' are often used interchangeably.
Traditionally, endometrial cancer was classified according to histologic features into type I (more common, lower-risk, estrogen-driven) and type II (less common, more aggressive, non-estrogen-driven). However, this classification method failed to fully capture the cancer's complexity. The World Health Organization and the International Federation of Gynaecology and Obstetrics (FIGO) have since developed classifications that include molecular features for more objective, reproducible categorization.
Endometrial cancers occur most frequently in high-income countries, with Europe ranking second among continents in the rates of both incidence and mortality in 2020. In 2022, approximately 130,051 women in Europe were diagnosed with endometrial cancer, with 29,963 associated deaths. Data from 2022 show that endometrial cancer‘s incidence is highest in Central Europe and mortality is highest in Central and Eastern Europe. However, the outlook for women diagnosed with endometrial cancer in Europe is relatively good, with nearly 80–85% surviving five years after diagnosis.
For more information on uterine cancer download the ENGAGe brochure What is uterine cancer (2024 update), or Gynaecological cancers in Europe (2024 update).
Symptoms
Signs and symptoms of endometrial cancer may include:
- Vaginal bleeding after menopause
- Vaginal bleeding between periods
- Light bleeding and a watery discharge, which may get heavier over time
- Pain in the back, legs or pelvis
- Diarrhoea or severe constipation
Risk factors
There are few risk factors for endometrial cancer, including:
- Older age
- Obesity and metabolic syndrome (diabetes with high insulin level)
- Never having been pregnant
- Family history
- Genetic predisposition
A small percentage of cases are associated with a specific familial syndrome (Lynch Syndrome) which is hereditary and can be inherited from parents/relatives. This syndrome also increases the risk of colorectal, ovarian and other cancers.
Risk factors for endometrial cancer include:
- Older age
- Obesity and metabolic syndrome (diabetes with high insulin level)
- Never having been pregnant
- Family history
- Genetic predisposition
A small percentage of cases are associated with a specific familial syndrome (Lynch Syndrome) which is hereditary and can be inherited from parents/relatives. This syndrome also increases the risk of colorectal, ovarian and other cancers.
Diagnosis
If one of the above-mentioned symptoms occurs regularly, ask your doctor.
To diagnose endometrial cancer, your doctor will first do a general examination, followed by further testing if necessary.
1) General examination (e.g., lymph nodes, abdomen, extremities)
• Vaginal examination, bianually including inspection of the cervix
• Transvaginal ultrasound to examine endometrial thickness, the cavity, the size and form
of the uterus, the ovaries and the rectouterine cul-du-sac
• Transabdominal ultrasound of the kidneys, liver, spleen (and check for free fluid)
2) If cancer or pathological findings are suspected, then further tests are necessary:
• Hysteroscopy: The doctor examines the womb with a camera. This procedure can be done without
anaesthesia as an “Office Hysteroscopy” or under sedation / light sleep
• Biopsy: It is necessary to take a probe of the endometrial layer by removing tissue with a curettage;
this can also be done with new small instruments (e.g., pipelle curettage or office hysteroscopy)
• In some cases, further imaging is indicated, including computer tomography, or magnetic resonance
imaging as well cystography and/or rectoscopy.
In the case of invasive diagnostics, the probe will be seen by a pathologist under a microscope.
Treatment
Treatment for endometrial cancer depends on the patient's age and general health and the stage and the grade of the tumor.
A physician will discuss options and possible adverse effects with you.
The options include the following options or a combination:
- Surgery
- Radiation therapy
- Chemotherapy
- Hormone therapy



